Two Merck drugs for treating male baldness and enlarged prostate will now carry extended labels to add more possible sexual side effects, US regulators said.
Month: April 2012
Lab-Grown Egg Cells Could Be ‘Fertilized Within the Year’ if License Is Granted
Researchers are now intending to seek permission from the Human Fertilization and Embryology Authority (HFEA) to fertilize the eggs in order to test whether they are viable. Should such a study be successful, it would represent a breakthrough in fertility research and could open the door to greatly enhanced fertility for many women.
What Is Polycystic Ovary Syndrome
- Irregular or skipped menstrual periods
- Obesity and difficulty controlling weight gain
- Male pattern hair growth
- Acne and other chronic skin conditions
- Dark brown or black patches on the skin
Polycystic Ovary Syndrome and Infertility
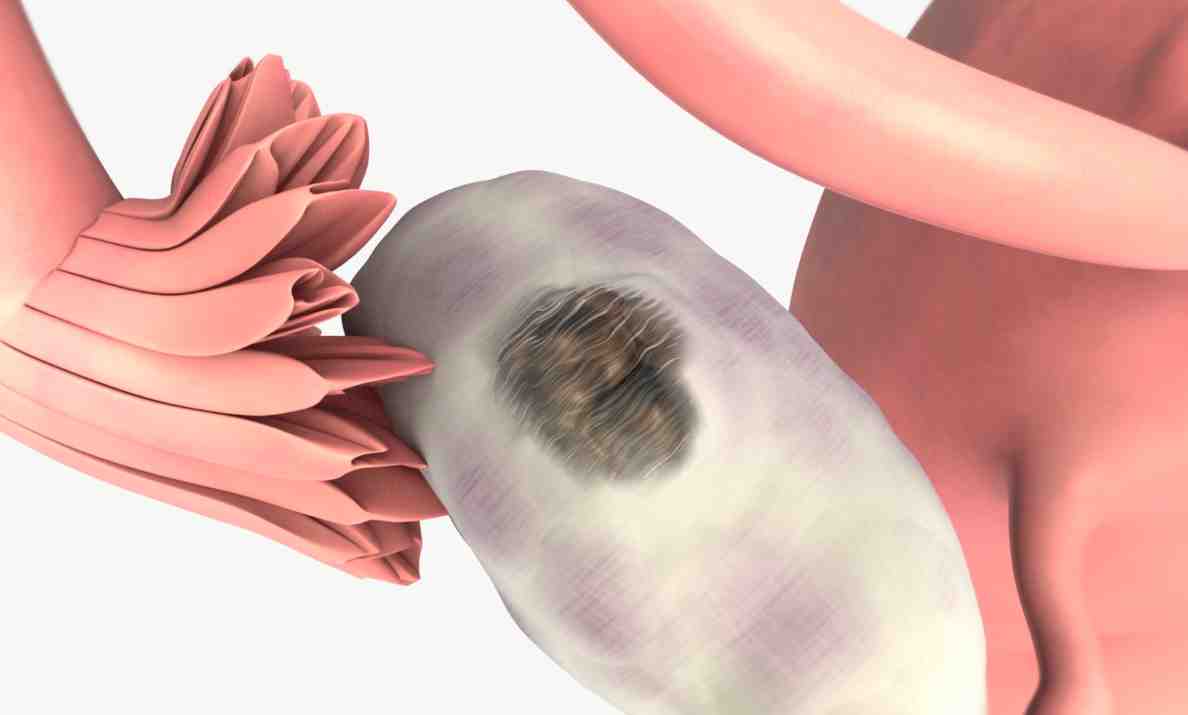
PCOS is the most common hormonal abnormality causing infertility in women. It affects fertility by suppressing ovulation. Egg follicles may begin to mature but do not ovulate or release the egg into the fallopian tube. These follicles remain as cysts in the ovaries. In women with PCOS, the ovaries also produce excessive amounts of testosterone (male hormone) that can lead to acne and hair growth. In the fat cells, testosterone is converted to estrogen, leading to excessive buildup of the uterine lining which may contribute to heavy or irregular bleeding.Fertility Treatment for PCOS
High levels of insulin associated with obesity interfere with ovulation and also worsen PCOS symptoms. Minimizing insulin resistance via a healthy, safe weight loss regimen is a common first step for patients with PCOS who want to make conception more likely. Insulin regulating medications may also be prescribed. Some women are able to begin ovulating more normally at this point and may be able to conceive naturally.Fertility enhancing drugs such as Clomid, Metformin and gonadotropins may be used to stimulate ovulation. This approach is tried after other potential causes of infertility have been ruled out. In-Vitro-Fertilization can also be used for some women with PCOS. by: Dr. John Jain
Surrogacy Experts Help Navigate Murky Legal Waters
According to the Society for Assisted Reproductive Technology, more than 1,400 U.S. babies were born this way in 2010, and many more such births are thought to go unreported. This small, but fast-growing field is fraught with risk, and often intense coordination is the only way to avoid a legal nightmare.
Who Is a Parent? Surrogate Technology Outpaces Law
Technology means someone who never thought they’d be able to conceive can use a sperm donor, an egg donor and a surrogate — a woman who bears a child for someone else. But the law has not kept pace with technology, and with so many people involved, a key question remains: Who is a legal parent?
Gel to Boost Male Fertility Being Developed
Male fertility has been largely overlooked until recently with most treatments requiring women to take medication or undergo expensive and invasive procedures.
Infertility Terms You Should Know
If you are seeking fertility treatment, you will hear many new words you may not be familiar with. The following are infertility terms you may need to know to fully understand your treatment options:
Aneuploidy – An abnormal chromosome count. This is an indication of serious defects in a fertilized egg that usually lead to early miscarriage.
Artificial Insemination – Introduction of sperm into a female patient’s reproductive tract through means other than intercourse.
Basal Body Temperature – The low body temperature reached after a night of sleep before a person gets up and begins moving around. A slight increase in this temperature usually occurs upon ovulation.
Basal Body Temperature Charting – Recording each daily temperature, plotted onto a graph in order to ultimately recognize a pattern. Your body temperature can rise gradually, suddenly or in steps. These patterns can differ from cycle to cycle.
Clomiphene Citrate (Clomid) – Clomid is a drug that stimulates ovulation by increasing production of gonadotropins (pituitary gland hormones). This is a commonly prescribed medication for infertility that involves menstrual cycle irregularities.
Egg Donation – Young women who wish to assist an infertile couple in achieving a pregnancy may undergo a course of hormone injections to stimulate a large number of eggs to mature at once. These donated eggs are retrieved and may be used immediately or frozen.
Egg Retrieval – Eggs are removed from a patient’s ovaries for use in vitro fertilization. This outpatient procedure involves the use of a long needle inserted through the vaginal wall to suction the eggs from the ovaries.
Embryo – A fertilized egg is referred to as an embryo until about week 8 of gestational development. After this, the term fetus is used instead of embryo.
Embryo Biopsy – A diagnostic test used to identify chromosomal abnormalities. This procedure is done by removing a single cell from an embryo that is developing in an IVF dish. The biopsy does not interfere with normal development.
Embryo Cryopreservation – Freezing of fertilized eggs for future use. This step sometimes allows multiple IVF attempts to be carried out from a single follicle stimulation/egg retrieval cycle.
Embryo Transfer – Introducing embryos that have developed for several days in an IVF dish into a woman’s uterus. The embryos are transferred via a flexible tube inserted through the cervix.
Endometriosis – A painful medical condition that causes abnormal growth of endometrial tissue (the type of tissue that lines the uterus). Endometriosis can cause fallopian scarring and other issues that lead to infertility
Fibroid – A non-cancerous tumor that grows on the wall of the uterus. Fibroids can occasionally interfere with fertility.
FSH Injections (Gonadotropins) – Follicle Stimulating Hormones trigger the maturation of eggs in the ovaries and make them ready for retrieval. These hormones are injected just under the skin.
Gender Selection – Selection of the desired gender either through sperm sorting or the much more accurate method of inspecting a developing embryo prior to transfer into the uterus.
Hydrosalpinx – Blockage of the fallopian tube with a clear liquid that prevents the passage of an egg and results in infertility. This medical condition is typically caused by infection with an STD that damages the fallopian tube at the end nearest the ovary.
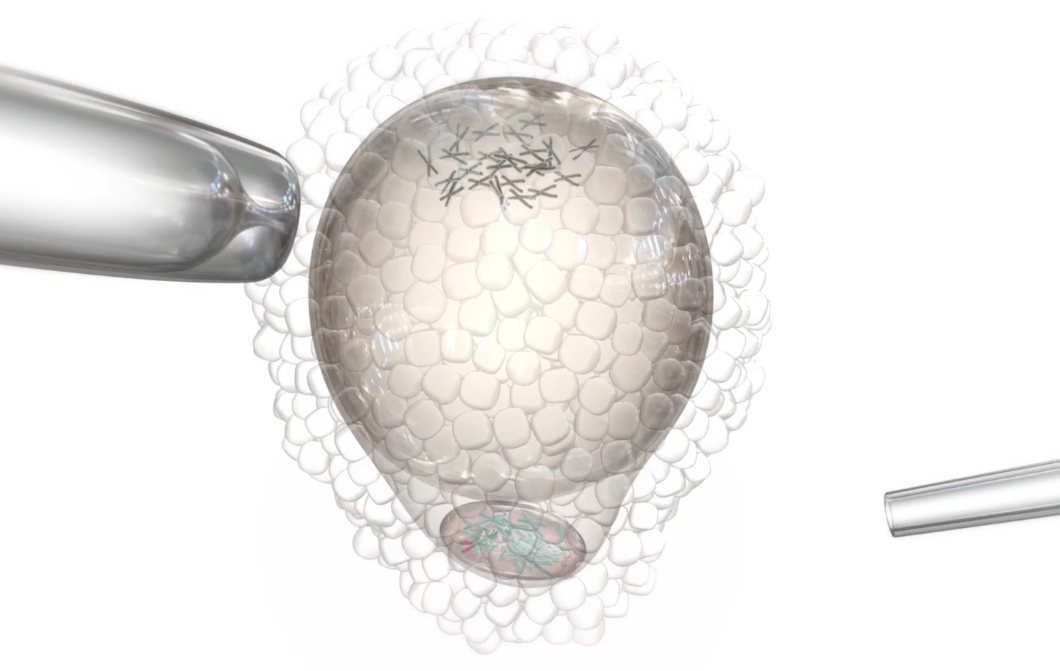
Intracytoplasmic Sperm Injection – Injection of a single sperm directly through the protective outer shell of an egg into the cytoplasm. The fertilized egg is kept in the IVF dish and observed to ensure fertilization and normal development before transfer.
Intrauterine Insemination – Sperm is collected from the male partner and processed to remove the semen components and concentrate the sperm. This sample is introduced into the female partner’s uterus. From there, the sperm travels to the fallopian tubes to fertilize an egg.
In-Vitro Fertilization – Sperm are introduced into an IVF dish that contains an egg so that fertilization occurs outside the patient’s body. The term In-Vitro Fertilization is often used to refer to the whole cycle of follicle stimulation, egg retrieval, fertilization, and transfer into the uterus.
MESA – Micro Epididymal Sperm Aspiration is a surgical procedure performed to retrieve sperm from the duct that stores sperm as it matures. It involves making a very small incision in the scrotum.
Oocyte Cryopreservation – Retrieval, freezing, and storage of a woman’s eggs for use in future fertility treatment.
Ovarian Reserve – The number of viable eggs a woman has remaining.
Ovulation – Release of a mature egg from the ovary into the fallopian tube where it can be fertilized. This normally happens once every 28 days about halfway through each menstrual cycle.
Ovulation Monitor – A device that measures hormones in the urine, sweat or other body fluids to determine when an egg is about to be released and can be used to pinpoint the best days for intercourse to achieve pregnancy.
Polyp – Excessive growth of endometrial tissue on stalks protruding from the lining of the uterus into the uterine cavity. These may cause miscarriage.
Pre-Implantation Genetic Diagnosis – Genetic screening of embryos for abnormal chromosome counts or mutations while they are developing in an IVF dish. PGD increases the success rate of IVF by detecting and screening out any embryos that cannot survive.
Semen Analysis – Evaluation of a semen sample to determine if the number, movement, and shape of a male partner’s sperm are normal.
TESE – Testicular Sperm Extraction is a surgical biopsy technique used to retrieve viable sperm from the testicles of men who cannot give a sperm sample by other methods.
Varicocele – A varicose vein occurring in the scrotum. When the valve in the vein fails, blood accumulates causing the vein to swell – potentially affecting fertility.
Vasectomy Reversal – Surgical reconnection of the vas deferens (ducts that carry sperm from the testicles to the point where the sperm is mixed with semen). This procedure may be used to restore normal fertility to a male partner.
Zygote Intrafallopian Transfer – Placement of a newly fertilized egg (zygote) directly into the fallopian tube. Returning the egg to its natural environment increases the chances of successful development and implantation.
Genetic Testing on Eggs Prior to Freezing
Eggs are more prone to genetic abnormalities as a woman ages. These abnormalities lead to increased incidences of infertility, miscarriage and birth defects especially in women over 38 years of age. Egg freezing is a method that suspends egg aging. Since the genetic status of an egg cannot be determined solely on appearance, methods to evaluate eggs using genetic probes have developed and recently tested.
The egg discards DNA at two different times during its development, ovulation and fertilization. The reason for this is to reduce the number of chromosomes to 23 in order to match the 23 chromosomes delivered by the sperm. The discarded DNA (in the form of excess chromosomes) is jettisoned outside of the egg as a small, round pocket called the polar body. Removal of the polar body (biopsy) can provide useful information about the genetic status of the egg. For example, if 23 chromosomes are found in the polar body, the presumption is that a normal count of 23 chromosomes remains in the egg. In contrast, if a number other than 23 is found in the polar body, it implies that an abnormal count remains in the egg and suggests that the egg and ensuing embryo will be genetically abnormal. Testing of the polar body using modern genetic techniques such as Comparative Genomic Hybridization (CGH) or Array-CGH, allows identification of abnormal eggs and can thus help determine the number of genetically normal eggs a woman has to freeze.
However, there are several important limitations to this technology. First, CGH and Array-CGH are still considered experimental, with very little clinical data available. Most clinical data is based on young egg donors and does not reflect the genetic status of eggs from women in their late 30’s. Second, embryos may be genetically abnormal due to mistakes contributed by the egg at the time of the first polar body formation or the second polar body formation; or mistakes contributed by the sperm at the time of fertilization. Therefore, assessing only the first polar body by no means guarantees that a normal embryo will derive. Third, and perhaps most concerning, is the lack of research regarding the effects of biopsying an egg prior to freezing.
We recently completed a small clinical trial wherein we performed polar body biopsy on eggs prior to freezing. We found a high degree of egg damage. The panel of microscopic pictures above demonstrate these changes: the first picture is a normal egg with an intact first polar body (Photo #1); the next picture is an egg after the polar body was removed (Photo #2); the next two pictures show a biopsied egg after freezing and thawing demonstrating egg contents (Photos #3 & #4) extruding through the biopsy slit. 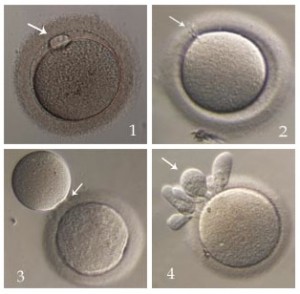 These changes were found on multiple eggs from different patients. These eggs had to be discarded. In addition, many other eggs demonstrated abnormal chromosome segregation after fertilization, and none of the patients achieved a pregnancy.
These changes were found on multiple eggs from different patients. These eggs had to be discarded. In addition, many other eggs demonstrated abnormal chromosome segregation after fertilization, and none of the patients achieved a pregnancy.
At the current time we do not recommend polar body biopsy of eggs prior to freezing until further studies on effectiveness and safety are available.
Why aren’t more young cancer patients preserving their fertility?
The answer to the question above, according to a recent study in the journal Cancer, is that too often, young women who have cancer simply don’t understand their options when it comes to preventing the loss of their chance to have a child or more children. According to Reuters Health, which reported on the new research late last month, only one in every 25 women who was diagnosed with one of five types of cancer since the early 1990s opted to freeze eggs or embryos prior to cancer treatment — in spite of the fact that 47 to 63 percent said they wanted to have a child or children.
This finding is the result of research on 1,000 women in California ages 18 to 40 who’d been diagnosed with cancer between 1993 and 2007. Sixty-one percent of the women said their doctors talked to them about how cancer treatment could affect their chances of having a baby and how they could preserve their fertility — which means that 39 percent of patients didn’t get that guidance. Just four percent of those who got counseling about fertility preservation took action – by freezing eggs or embryos before, say, they underwent chemotherapy or radiation.
The research found, not surprisingly, that the women who had been counseled about how to save their fertility, or minimize the impact of treatment on their ability to conceive, were much less likely to feel regret later, versus the women who’d never talked to a doctor about their options for having a child or children later before undergoing treatment. Though the most recent data is still five years old, there’s reason to believe we still have a bit to go before all young women who get a cancer diagnosis are aware of all their options for having a family as they consider the treatment plan that’s right for them.
Study: Egg Donors Remain Fertile After Procedure
Some experts question whether hormonally stimulating the ovaries — which makes them produce extra eggs — and removing those eggs from a healthy, young woman could later increase her chance of infertility, but others contend there are no serious long-term risks.